Monkeypox
Table of Contents
ToggleKey Facts
- Monkeypox is a viral infection caused by the monkeypox virus, a member of the Orthopoxvirus genus in the family Poxviridae.
- The monkeypox virus is a zoonotic disease prevalent primarily in the tropical rainforests of Central and West Africa, although it is occasionally transmitted to other parts of the world as well.
- The main symptoms of monkeypox are fever, rashes, and swollen lymph nodes and it may also cause some medical complications.
- The symptoms of monkeypox usually last between two and four weeks. The situation can become severe in some cases. Recent case-fatality ratios have hovered around 3-6%.
- Humans can become infected with monkeypox by coming into contact with infected people, animals, or contaminated material.
- The monkeypox virus is spread through close contact with lesions, body fluids, respiratory droplets, and contaminated bedding. Monkeypox resembles smallpox, an orthopoxvirus infection that was eradicated worldwide in 1980.
- Unlike smallpox, monkeypox causes less severe illness and is less contagious.
- Smallpox vaccines provided protection against monkeypox as well.
- In recent years, new vaccines have been developed for the prevention of monkeypox, one of which has been approved for use.
- A smallpox antiviral agent has also been approved for monkeypox treatment.
Introduction
As a viral zoonosis (a virus transmitted from animals to humans), monkeypox has clinical symptoms very similar to those of smallpox patients in the past, though it is less serious. Monkey pox has emerged as the most important orthopoxviral for public health since smallpox was eradicated in 1980. Primarily found in Central and West Africa, monkey pox has become more common in urban areas, especially near tropical rainforests. Non-human primates and rodents are the main animal hosts.
The pathogen
Monkeypox virus is a double-stranded enveloped DNA virus and comes under the Orthopoxvirus genus of the poxviridae family. The Central African (Congo Basin) clade and the West African Clade are the two distinct genetic clades of the monkeypox virus. It is the congo basin clade that has caused more severe diseases than the West African Clade and it is believed to have more transmission rate. Cameroon is the only country in the world where both the virus clades have been found.
Natural host of monkeypox virus
Various animal species have been found as the natural hosts of the monkeypox virus. Some of these species are rope squirrels, tree squirrels, Gambian Pouched Rats, dormice, non-human primates and other species. The history of the monkeypox virus is still perfectly unknown and research are going on based on this topic.
Outbreaks
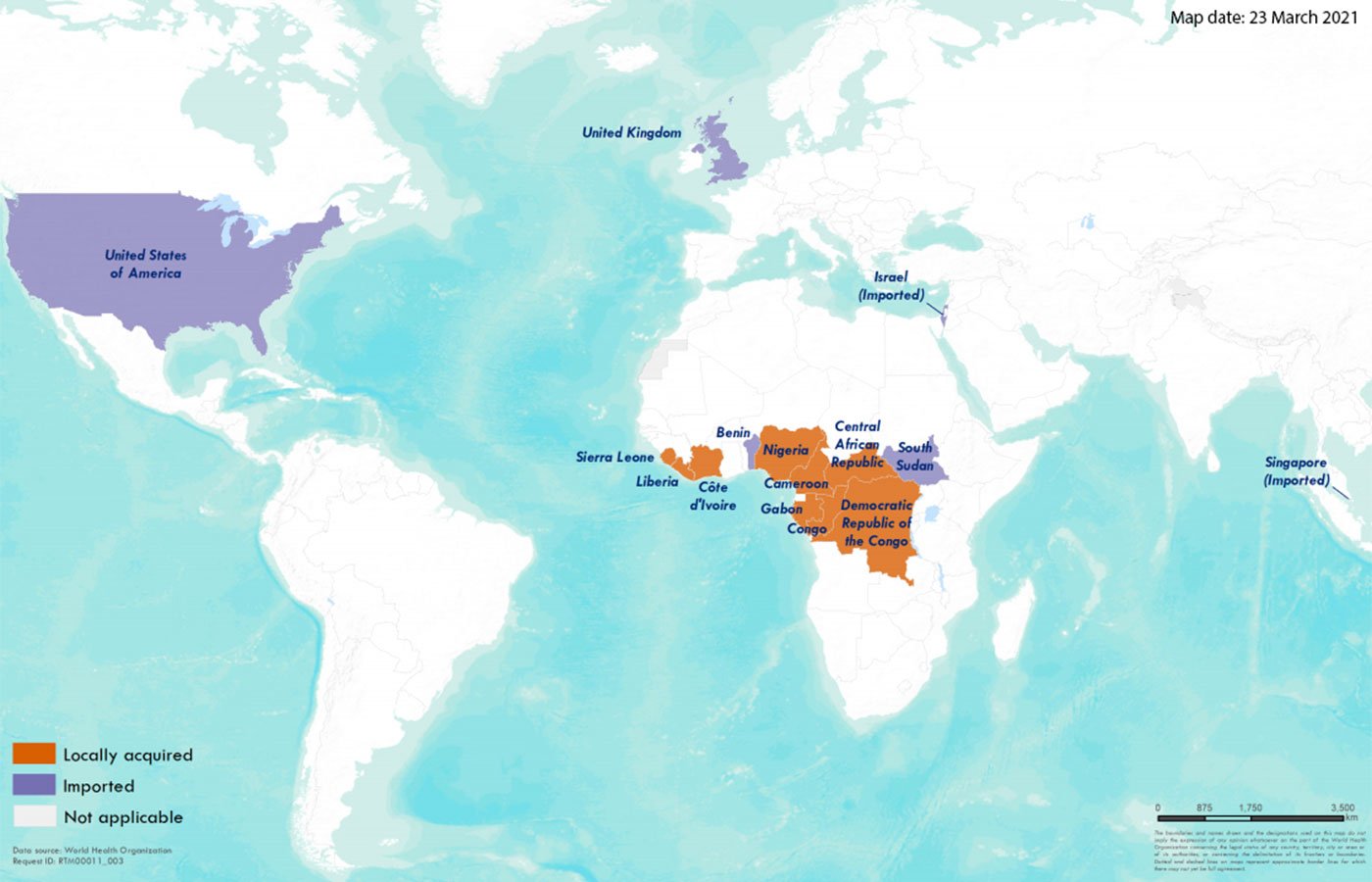
Monkeypox virus was first found in humans in 1970 in the Democratic Republic of Congo. The virus was first declared in a 9-year-old boy in the same place where smallpox has been eradicated in 1968. Since then, most monkeypox cases have been reported in Central and West Africa.
After its declaration in 1970, Monkeypox has been reported in 11 African nations including Benin, Cameroon, the Central African Republic, the Democratic Republic of Congo, Gabon, Cote d’Ivoire, Liberia, Nigeria, Sierra Leone, and South Sudan. The true burden of this disease is not known. For example, a monkeypox outbreak occurred in the Democratic Republic of Congo in 1996-97 and this outbreak had less fatality ratio but a higher attack rate. Its Nigeria that has reported more monkeypox cases since 2017 with over 500 suspected cases and over 200 confirmed cases. The fatality ratio is approximately 3%. The cases are reported even today.
The first monkey pox outbreak outside Africa was reported in the US in 2003. It is believed that the disease reached US through infected pet prairie dogs. These dogs had contact with Gambian pouched rats and dormice imported to US from Ghana. 70 monkeypox cases have been reported in the US in this period of time. In some instances, travellers from Nigeria became monkeypox carriers and spread the disease to Israel in September 2018, to the United Kingdom in September 2018, May 2021, and May 2022, to Singapore in May 2019, and to the US in July and November 2021. Multiple cases of monkeypox were reported in several non-endemic countries in May 2022. Studies and research are presently going on to trace the epidemiology, sources of infection, and transmission patterns.
Transmission
Zoonotic transmission, i.e., animal-to-human transmission can take place through direct contact with the blood, bodily fluids, or cutaneous or mucosal lesions of infected animals. In Africa, the monkeypox virus has been found in animals like rope squirrels, tree squirrels, Gambian Poached Rats, dormice, several species of monkeys, and so on. The natural source of monkeypox is not yet known, but rodents are more suspected. Monkeypox may also spread through consuming the meats of infected animals.
Close contact with respiratory secretions, skin lesions of an infected person or recently contaminated objects can lead to human-to-human transmission. Other people at the highest risk are health workers, family members and close contacts of the patient as they are spending more time with them and transmission through droplet respiratory particles is also possible. In recent years, the longest documented chain of transmission in a community has increased from six to nine successive person-to-person infections. As cessation of the smallpox vaccine is going to occur, this may lead to less immunity in all the communities. Another possible way of transmission is from the placenta of the mother to the fetus or via close contact during and after birth. Many diseases are transmitted through sexual contact but in the case of monkeypox, the possibility of transmission through sexual contact is not yet clarified. Studies related to this matter are currently going on.
Signs and symptoms
The incubation period of monkeypox ranges from 6 to 13 days, but in some cases, it may be 5 to 21 days.
The infection comprises two periods,
The first one is the invasion period during which fever, intense headache, lymphadenopathy, back pain, myalgia (muscle aches) and intense asthenia (lack of energy) occurs. Compared to other diseases like chickenpox, measles, smallpox etc., lymphadenopathy is a distinctive feature of monkeypox infection.
The skin will start to break down within 1-3 days of the appearance of the fever. Rashes will appear on your body and it mainly comes on your face and related parts rather than your trunk. The rashes also affects other parts of the body but in 95% of the cases it affects the face. The rashes starts to develop from the macules (lesions with a flat base) to the papules (slightly raised firm lesions), vesicles (lesions filled with clear fluid), pustules (lesions filled with yellowish fluid), and crusts that dry up and fall off.
The symptoms of monkeypox lasts from 2 to 4 weeks. Serious cases of monkeypox mostly occur in children. The severity of the infection depends on the virus exposure, patient’s immunity capability, and nature of complications. Monkeypox may also lead to secondary infections, bronchopneumonia, sepsis, encephalitis, and cornea infection that may lead to loss of vision.
The overall fatality ratio of monkeypox is 0-11% in the general population and this has been higher among children. Recently, the fatality ratio ranges from 3-6%.
Diagnosis
It is important to consider other rash illnesses, such as chickenpox, measles, bacterial skin infections, scabies, and syphilis, as well as allergies caused by medication. Lymphadenopathy during the prodromal stage of illness can be a clinical feature to distinguish monkeypox from chickenpox or smallpox.
To confirm monkeypox, a sample should be collected and transportedory.
Laboratory tests and specimen quality determine whether monkeypox has been confirmed. National and international standards should be followed when packaging and shipping specimens.
PCR is the most accurate and sensitive laboratory test available. A good diagnostic sample for monkeypox would be the roof or fluid from vesicles or pustules, or dry crusts. In cases where biopsy is feasible, it should be considered. A dry, sterile tube with no viral transport medium must be used for storing lesion samples. Patients should not routinely be tested for viremia through PCR blood tests due to the short duration of viremia relative to the timing of specimen collection after symptoms begin.
Due to the serological cross-reactivity of orthopoxviruses, antigen and antibody detection do not provide monkeypox-specific confirmation. It is therefore not recommended to use serology or antigen detection methods for diagnosis or case investigation where resources are limited. Vaccination with a vaccinia-based vaccine (e.g. anyone vaccinated before smallpox eradication or more recently vaccinated due to higher risk such as orthopoxvirus laboratory personnel) might result in false positive results as well. Test results can only be interpreted if accurate patient information is included with specimens, such as: a) the date the patient developed fever, b) the date the individual developed rash, c) the date of specimen collection, d) the individual’s current medical status (stage of rash), and e) their age.
Therapeutics
Monkeypox should be treated with full optimization of clinical care to relieve symptoms, manage complications, and prevent long-term effects. Fluids and food should be offered to patients to maintain an adequate nutritional status. Infections caused by secondary bacteria should be treated according to their severity. Based on animal and human studies, tecovirimat, which was initially developed for smallpox, was licensed by the European Medical Association (EMA) for monkeypox in 2022. Still, it is not widely available.
Vaccination
It is found that the smallpox vaccine is 85% effective against monkeypox. But the issue is that smallpox virus is no longer available to the public. In 2019, a vaccine has been developed for monkeypox based on a modified attenuated vaccinia virus, the Ankara Strain. This vaccine consists of two doses but its availability is limited. There is cross-protection provided for the immune response to orthopoxviruses by smallpox and monkeypox vaccines based on vaccinia virus.
Prevention
As a perfect vaccine is not available for monkeypox, protecting yourselves is the main way to get away from this dreaded infection. Have a healthy bath, use mask and sanitizers like you are protecting yourselves from the pandemic Covid 19 and always keep good cleanliness. It will be also good to give awareness about monkeypox to the public, give an idea to the public what monkeypox is, how it is caused, what are the after effects of the infection and how can you protect yourselves from the infection. This will surely enable people to get an overall idea about monkepox. Scientific research is presently going on to discover a perfect vaccine for monkeypox and lets hope for the best.
Reducing the risk of human-to-human transmission
The main issue during monkeypox outbreaks is people having close contact with infected ones. This may lead to serious consequences. So always avoid contact with infected people. People at high risk are health workers and household members as they are always treating and caring patients, thereby maintaining a close contact with them. To avoid this situation, people who already took the vaccine should be appointed to care the patients. This may reduce the risk of the infection.
In laboratories equipped with the appropriate equipment, samples taken from people and animals suspected of having monkeypox virus infection should be handled by trained personnel. In accordance with WHO guidelines, patient specimens must be transported safely in triple packaging.
Clusters of monkeypox cases were identified in several non-endemic countries without direct travel links to an endemic area in May 2022. A further investigation is underway to determine the likely source of infection and limit further spread. It is important to investigate all possible modes of transmission as the source of this outbreak is being investigated.
Reducing the risk of zoonotic transmission
As you know many cases of infection has been reported due to people having close contact with animals, i.e., through meat, blood, etc. People having meats of infected animals being the main reason for this. So, before having meat of a particular animal, don’t forget to cook it properly. This may save you from this serious threat.
Preventing monkeypox through restrictions on animal trade
There are some countries that restrict the importation of rodents and non-human primates. If captive animals are suspected to be infected with monkeypox, they should be quarantined immediately. Observe any animals that have come into contact with the infected animal for 30 days, take standard precautions, and quarantine them.
How monkeypox relates to smallpox
Monkeypox has similar clinical features to smallpox, another orthopoxvirus infection that has been eradicated. About 30% of patients who contracted smallpox died due to the ease of transmission and the severity of the illness. A global campaign of vaccination and containment resulted in the last case of naturally acquired smallpox occurring in 1977, and the disease was declared eradicated worldwide in 1980. All countries have stopped routine smallpox vaccination with vaccinia-based vaccines more than 40 years ago. Since vaccination also protects against monkeypox in West and Central Africa, unvaccinated populations are more susceptible to infection.
However, the global health sector remains vigilant in case smallpox recurs through natural mechanisms, laboratory accidents, or deliberate release. New vaccines, diagnostics, and antiviral agents are being developed in order to prepare for the reemergence of smallpox. Moreover, they might also prove helpful in the prevention and control of monkeypox.
Read more : Sexually Transmitted Diseases



